Practical Interpretation: Neurophysiological Monitoring Commonly Used in Spinal Surgery
Release date: 2016-10-13
The dancer on the tip of the knife, some people describe the spine surgeon. As a mid-axis bone, the spine has functions such as weight-bearing, shock absorption, protection, and exercise (Fig. 1), and the aging of society is accompanied by a marked increase in the incidence of degenerative diseases of the spine. Spinal degenerative diseases cause low back pain, shoulder and neck pain, and even movement disorders. Therefore, more and more patients need surgery to intervene.

Figure 1 Spinal anatomy (from the Nite - Human Anatomy Atlas)
However, the spinal cord in the spinal canal and the nerves it sends out make every spine surgeon feel thin. Even the clever dancers may make mistakes, and they are a little careless. As a spine surgeon, even if you have had hundreds of operations, you can only let the patient wake up and see that his hands and feet can move, and the hanging heart can be put down. Now, the emergence of neurophysiological monitoring, like a pair of platform shoes, provides a guarantee for spine surgeons. Let's take a look at the application of neurophysiological monitoring in spinal surgery.
Purpose and main methods [1-5]
The purpose of neurophysiological monitoring during spinal surgery is as follows [6] :
1. Feedback on changes in neurological integrity during surgery;
2. Take measures to avoid irreversible damage;
3. Reduce the risk of postoperative neurological deficits.
The main methods include:
1. Somatosensory evoked potentials (SEP): monitoring the function of the upstream sensory nerve conduction system;
2. Motor-evoked potentials (MEP) monitor the function of the descending motor nerve conduction system;
3. Electromyograph (EMG): monitors the function of the cranial nerve, spinal cord, and peripheral nerves that govern muscle activity.
Somatosensory evoked potential (SEP)
The primary function of SEP is to monitor the function of the upstream sensory nerve conduction system (Figure 2).
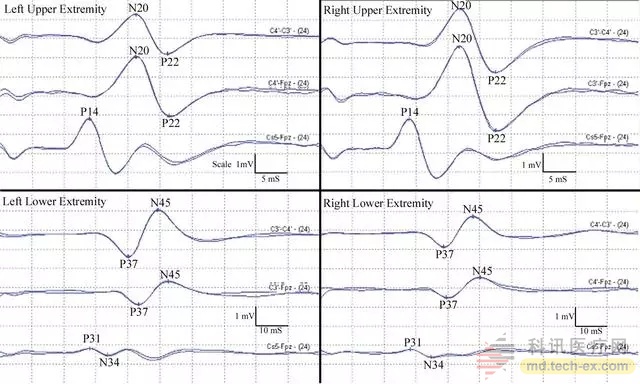
Figure 2 SSEP performance of normal median nerve and posterior tibial nerve (Image courtesy of Gonzalez, AA, et al., Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus)
The advantage is that the repeatability is good, the monitoring can be continuous, away from the surgical field, the impact on the surgery is small, and the operability is good. However, its shortcomings are also obvious: too many influencing factors can not be eliminated, including anesthesia, body temperature, mean arterial pressure, electrical interference, etc., which will affect the results, so the use is limited.
In a retrospective survey of 33,000 spinal cord surgery cases, the American Spinal Research Association found that 28% of neurological complications were not detected by SEP. Moreover, SEP reflects the time of spinal cord injury about 16 min behind MEP. SEP is also a multiple nerve root conduction. It is neither sensitive nor specific for the monitoring of nerve root injury, so it needs to be replaced by EMG monitoring.
Its main indicators of observation are latency and volatility. Early warning criteria: volatility drops by more than 50% and/or latency increases by more than 10%. Abnormal changes in SSEP for more than 10 min indicate a risk of neurological damage. Wave amplitude changes: <30% is a normal change; 30% to 50% requires close observation; >50% suggests nerve damage (Figure 3).
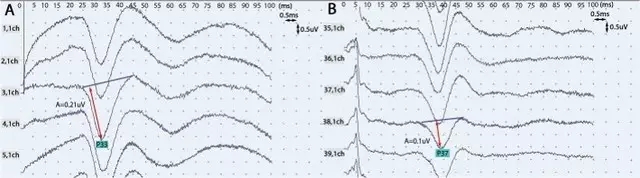
Figure 3 Figure A is the normal case, the amplitude is 0.21 uv, and the latency is 33 ms, while the amplitude in Figure B is 0.1 uv and the latency is 38 ms. As a result, the amplitude is reduced by 52.4% and the latency is extended by 12%, suggesting a risk of neurological damage.
Motor evoked potential (MEP)
The main function of the MEP is to monitor the function of the descending motor nerve conduction system.
The advantage is that it can directly and directly reflect the functional state of the motion conduction path. The main disadvantage is that the repeatability is worse than SSEP and may be affected by muscle relaxants.
The warning criteria are currently controversial, with or without criteria: only when the MEP disappears completely predicts postoperative dyskinesia.
Amplitude criteria: It is generally considered that a reduction of 80% of the amplitude of at least 6 times is considered a positive change. Others believe that a 50% reduction in volatility suggests a risk. Because individuals vary greatly, it is best to have a reference channel.
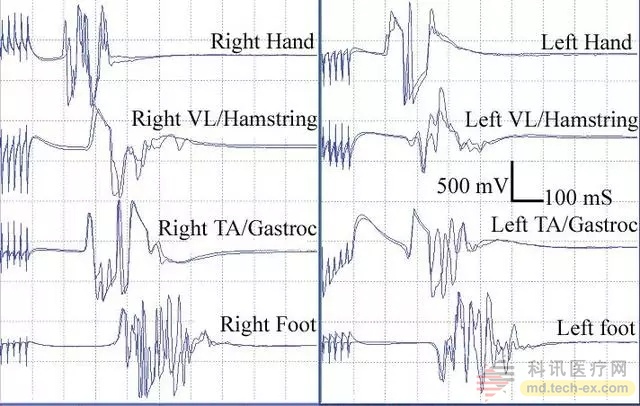
Figure 4 MEP manifestations of normal lateral femoral muscle, posterior muscle group, tibialis anterior muscle, gastrocnemius muscle (Image courtesy of Gonzalez, AA, et al., Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus)
Electromyography (EMG)
The main function of EMG is to monitor the nerve roots during spinal surgery, which is divided into spontaneous EMG and induced EMG (Figure 5).
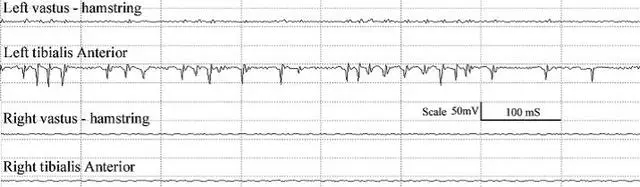
Figure 5 A series of activities of the tibialis anterior muscle during nerve root retraction
Spontaneous EMG refers to the electrical activity recorded on the muscles innervated by the nerve after stimulation of the intraoperative nerve. The continuously recorded information can promptly stimulate the stimulation of the nerve root. The basic principle of induced EMG is that if the screw is close to a nerve root, the screw will stimulate the nearby nerve root at a relatively low current and a compound action potential will appear.
The advantage is that it can monitor the nerve root condition in real time, and can help determine the position of the pedicle screw. The main disadvantage is that sensitivity and specificity are not high. The early warning standard is the outbreak of electrical activity (Figure 6); continuous long-term electrical activity lasts for a few seconds to a few minutes.
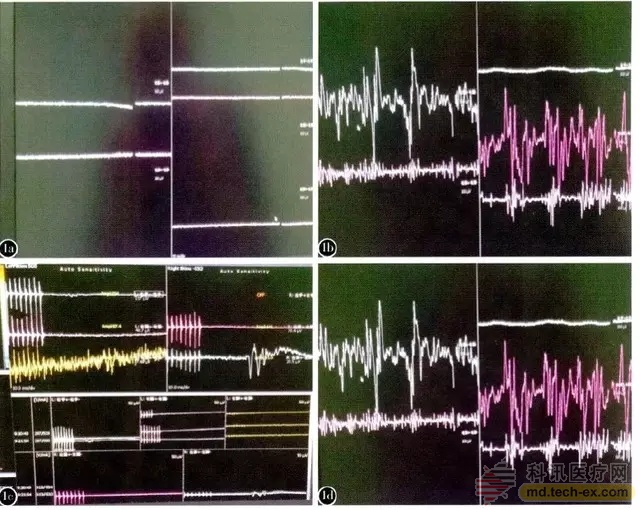
Figure 6 Electromyogram in XLIF, A is a normal spontaneous electromyogram, B is a spontaneous electromyographic electrical activity, suggesting that the nerve root is mechanically stimulated, and C is a normal EMG when pedicle screw fixation, D is Compound action potential, suggesting pedicle rupture
In addition, EMG can also be used to assess the position of the pedicle screw during surgery: EMG waveforms are derived when the stimulation power is ≤ 10 mA, indicating that the pedicle screw penetrates the pedicle cortex. When the EMG waveform is drawn at 10-20 mA, the pedicle screw may penetrate the cortex. When the stimulation volume is >20 mA, the EMG waveform is extracted, indicating that the pedicle screw is located in the pedicle cortex.
Therefore, the rational use of neurophysiological monitoring in spinal surgery can effectively reduce the risk of accidents and escort our surgery.
Author: Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Department of Orthopedics Li Sheng-jun
references
1. Avila, EK, et al., Intraoperative neurophysiologic monitoring and neurologic outcomes in patients with epidural spine tumors. Clinical Neurology and Neurosurgery, 2013. 115(10): p. 2147-2152.
2. Deletis, V. and F. Sala, Intraoperative neurophysiological monitoring of the spinal cord during spinal cord and spine surgery: a review focus on the corticospinal tracts. Clin Neurophysiol, 2008. 119(2): p. 248-64.
3. Rabai, F., R. Sessions, and CN Seubert, Neurophysiological monitoring and spinal cord integrity. Best Practice & Research Clinical Anaesthesiology, 2016. 30(1): p. 53-68.
4. Wang Wei, et al., Multi-mode neurophysiological monitoring in spinal surgery. Journal of Epilepsy and Neuroelectrophysiology, 2014. 23(5): p. 263-266.
5. Qiu Yong, Application of neurophysiological monitoring in spinal orthopedics. Chinese Journal of Medicine, 2015. 95(21): p. 1642-1643.
6. Gonzalez, AA, et al., Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus, 2009. 27(4): p. E6.
Source: Orthopedic time
Trifanz has a range of high quality anaesthetic face masks available in six sizes from neonate to large adult.
This Anesthesia Mask by Trifanz Medical can be used for anesthesia, respiratory or resuscitation use. Anesthesia mask features clear flexible faceplates with a contoured cushion that creates a gentle seal with the patient`s face. This disposable mask is meant for single-use only and has a universal fit connector. This cushion is a soft, pliable air-filled cushion that includes an inflation valve on the top and hook ring. This Anesthesia Mask is Non-sterile and Latex-free, using only high-quality, medical grade, clear PVC. This mask follows ISO standard sizing and is available in a range of sizes for adult, pediatric and infant use. Masks are individually bagged with color-coded rings for size identification.
The silicone anesthesia face mask can be repeated use and autoclaved at 134℃

Type: Horizontal Valve Anesthesia Face Mask, Valve Up Anesthesia Face Mask, Non Valve Anesthesia Face Mask, Siliocne Anesthesia Face Mask
Size: 0# Neonatal to 6# Adult XL
Anesthesia Face Mask,Air Cushion Face Mask,Reusable Silicone Anesthesia mask,Medical Disposable Anesthesia Mask
Hangzhou Trifanz Medical Device Co., Ltd , https://www.cfzmeds.com